→ AI Implemented
The Challenge
Walmart Pharmacy is one of the largest pharmacy chains in the United States serving millions of patients. Walmarts current fulfillment software lacks the ability to effectively and efficiently resolve common issues such as prior authorization and change requests. This inefficiency has lead to an unsustainable use of labor and and has dramatically attributed to patient attrition.
The Solutions
Given the size and complexity of the issues, we utilized several methods and tactics to achieve our goals. These included restructuring the current architecture, implementing limited automation, integrating outside services, redesigning the interface to reduce cognitive load and presenting conditional information to the user. In addition we also enhanced communication between patients and pharmacy staff in order to reduce patient attrition.
My Role
I was introduced to the project after the initial discovery and user interviews had occurred. I was tasked with researching and evaluating internal and external systems, conducting ideation sessions, assisting in interviews / user testing and creating wireframes / prototypes. I was also responsible for creating visual style and direction.
Research Methods & Results
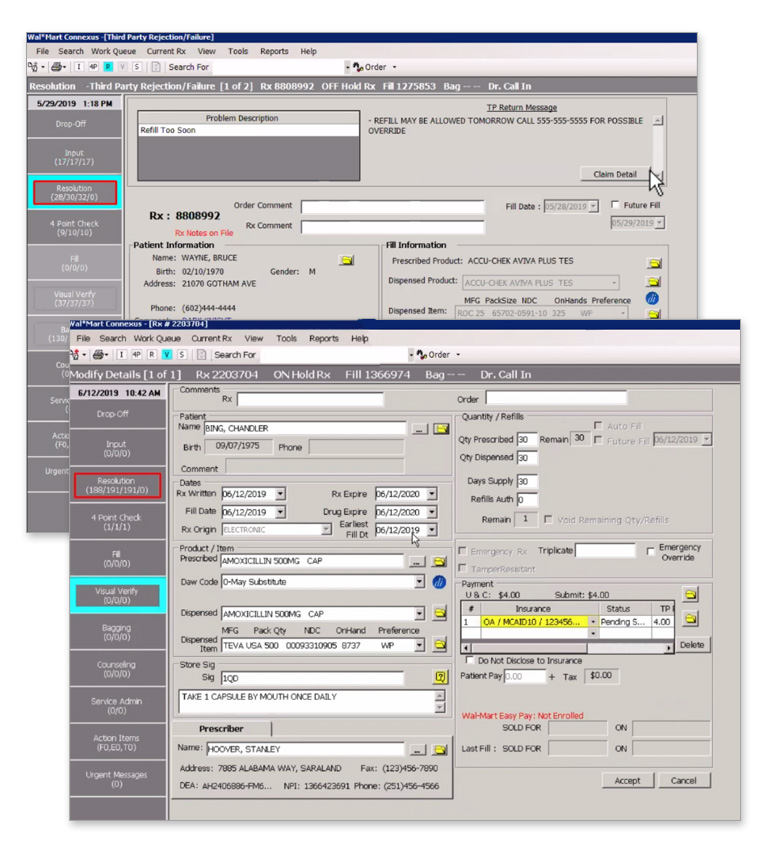
Observation
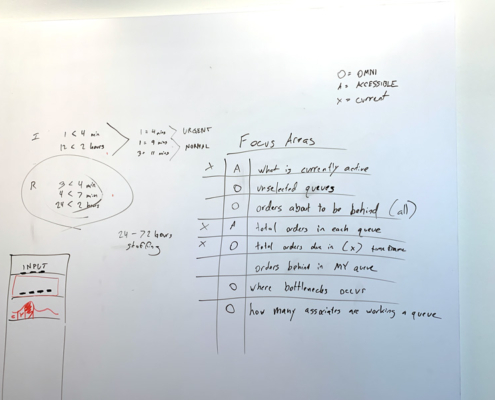
Over the course of several days our team members observed pharmacist and pharmacy techs processing patient prescription within Walmart’s test facility. This lead to several discoveries. Most of the pharmacy staff navigated through the system using F keys and rarely used a mouse to navigate. Users were also overburdened with tedious and inefficient processes with multiple popups, overbearing and frequent alerts as well as erroneous omni present information. Collectively this pointed to the system putting the users under unnecessary strain.
Interviews
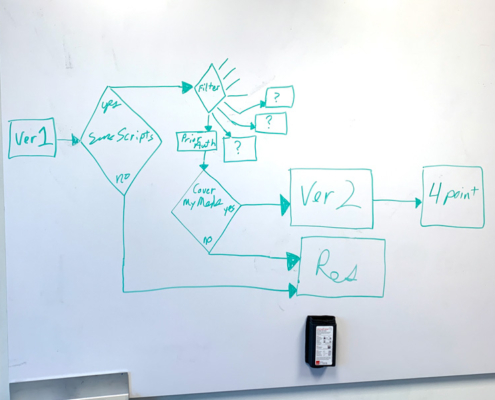
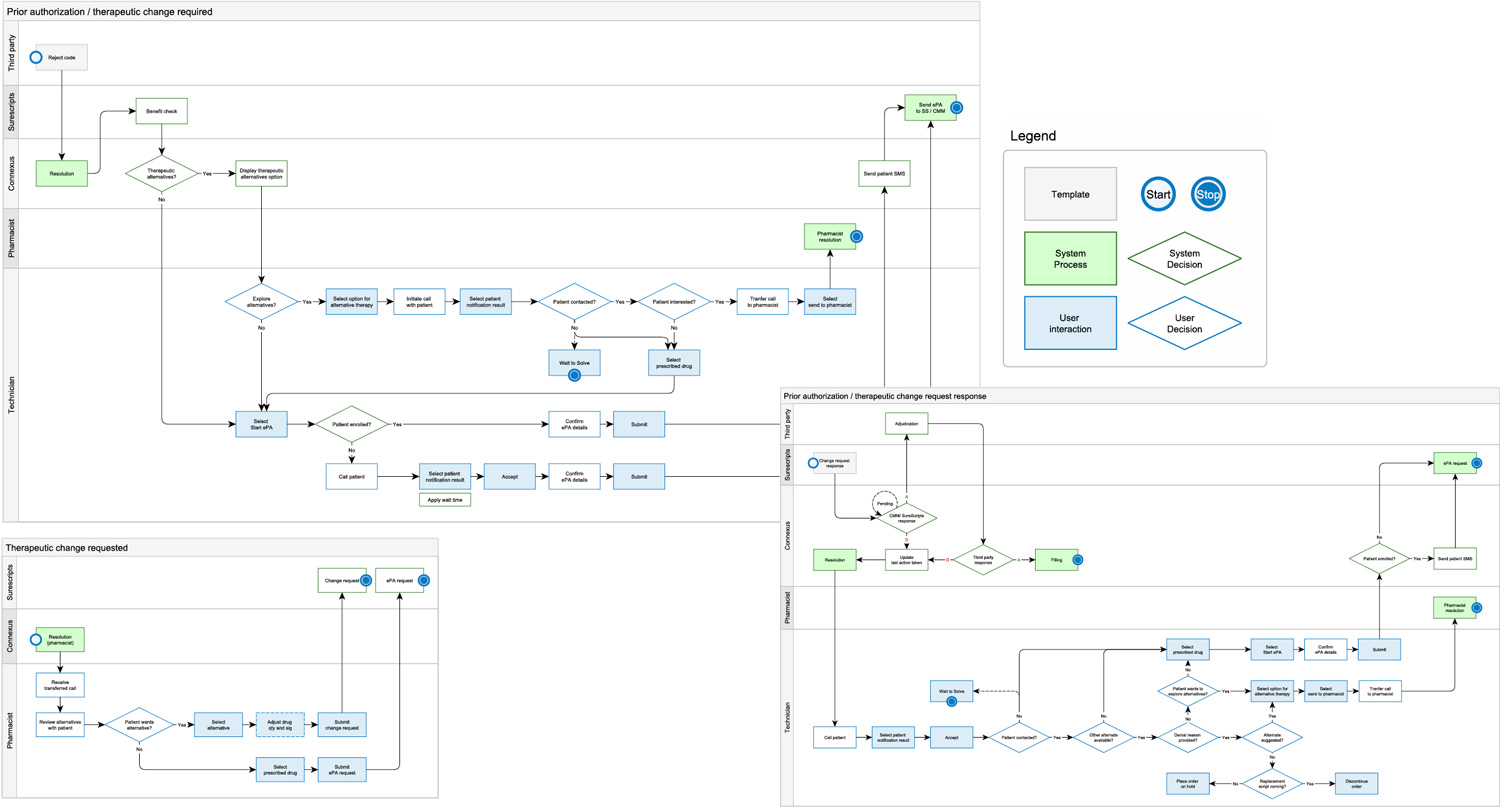
Our team conducted a multitude of interviews with pharmacist, techs, and stakeholders from several departments. This lead to the conclusion that the architecture needed to be restructured and outside processors such as Cover My Meds and Surescripts would be integrated. We also discovered that the communication between patients and pharmacy staff was inconsistent and often left patients in the dark whenever a prescription required a prior authorization or change request. This lack of communication lead to unmeasurable attrition and verbal conflicts between pharmacy staff and patients.
Usability Testing
Over the course of a 2 month period we worked in 2-3 day irritative cycles of user testing / interviews, ideation, and prototyping. During this period we developed a new intuitive interface, restructured multiple resolution processes, integrated outside processors, and enforced patient communication.
Synthesis Methods
Click Icons to View Details
Insights
Through our research we assessed that the current system created a tremendous amount of cognitive load on it’s users. This coupled with a patchwork of tacked on functions created an environment that was disorganized and confusing to navigate. This also led to a breakdown in communication between pharmacy staff and patients. We worked to resolve the issues in the following ways.
- Remap the current architecture
- Introduce outside processors ( Cover My Meds, Surescripts ) to speedup resolutions of prior authorizations and change requests
- Introduce automation where applicable
- Remove erroneous omni present information
- Present users with conditionally displayed info need to solve resolutions
- Create guided instruction though-out the resolution process
- Reduce the number of interactions needed to solve resolutions
- Modernize interface to reduce cognitive load
- Enforce patient communication
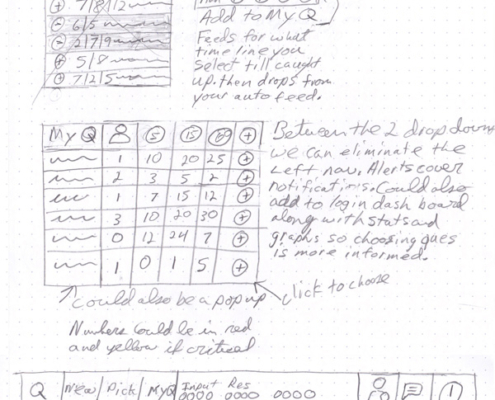
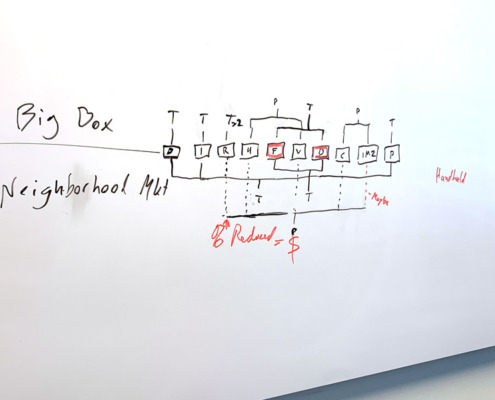
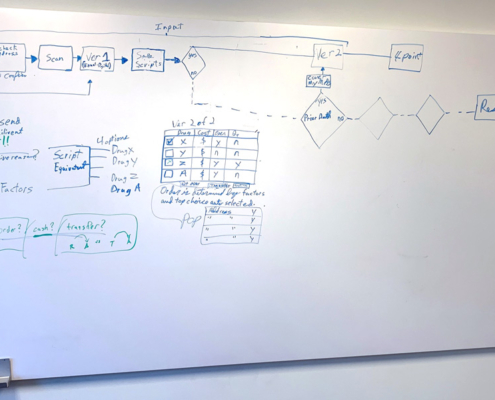
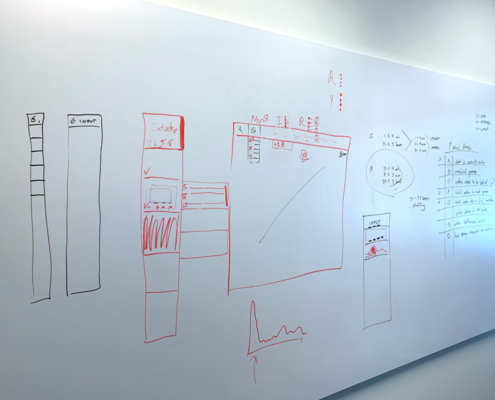
Conceptualization
Architecture
User Interface
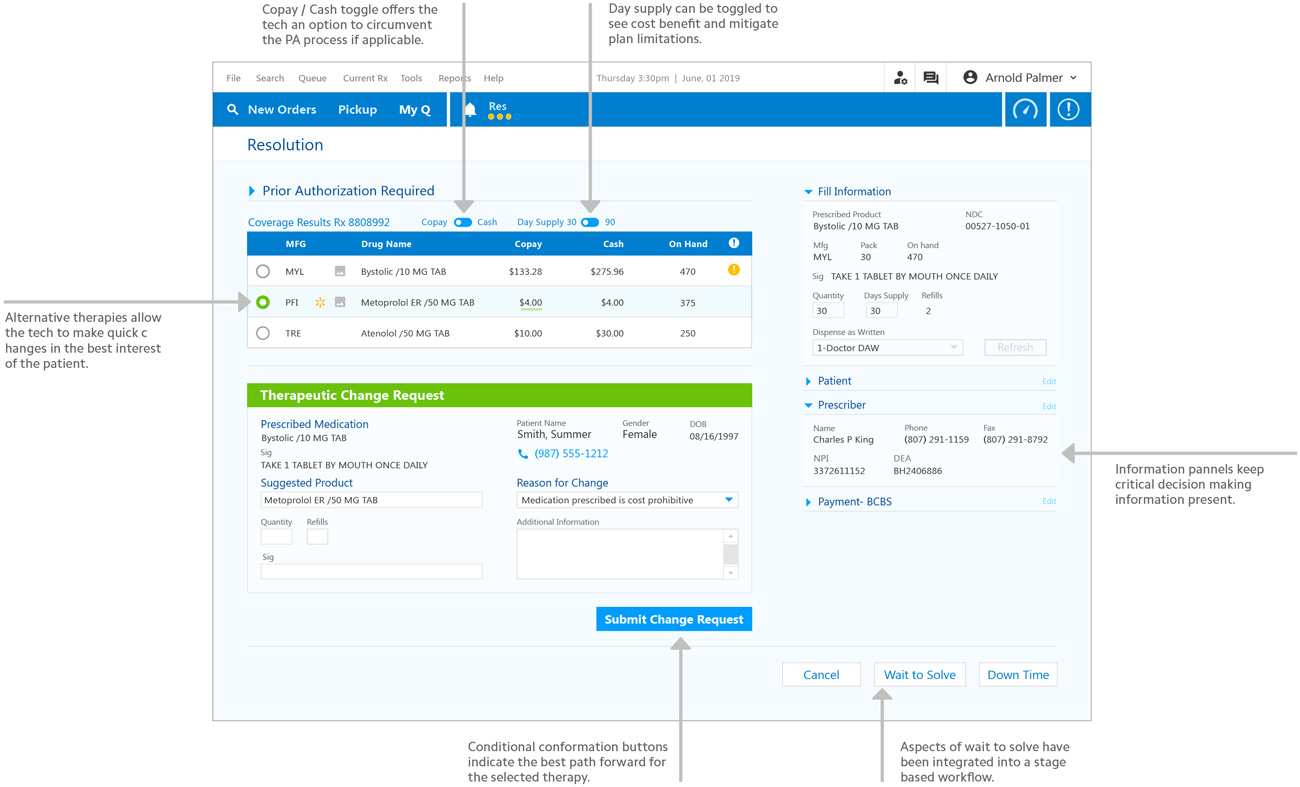
Streamlined Interface
Through a combination of reducing visual noise, giving a clear path, presenting conditional instructions and allowing for flexibility, we have created a solution that will reduce resolution time. This will result in a better experience for patients and pharmacy associates.
Key Benefits
- Integrated real-time benefit check
- Alternative therapy and pricing options
- Guided resolution instructions
- Enforced patient communication
- Enhanced tooling for quick changes
Workflow Consistency
Providing visibility into therapeutic options allows Technicians to make quick adjustments to avoid prior authorization delays. A consistent stage-based workflow between roles during the change request approval process promotes a seamless transition.
Key Benefits
- Workflow consistency between roles
- Pharmacist approval options
- Stage-based completion
- Automated order progression
Prototype
Click Image to Play
Results
73% Reduction
of touch points to solve resolutions
As a result of reducing the number of touch points from 15-20 down to 4 we have drastically reduced the amount of effort needed to resolve resolutions.
We have accomplished this by leveraging Surescripts and giving pharmacy staff a guided path with conditionally available information.
In addition, we have dramatically reduced the cognitive load on pharmacy staff. By cleaning up the interface and displaying consistent layouts, we have eliminated the need to hunt for information. As a result, Walmart’s operational and training requirements will also be reduced.